History & Background
Is a Blood Disorder?
Blood is made up of the following components :
Red Blood Cells :
Red Blood Cells (RBCs) give the red colour to blood. RBCs have a substance called haemoglobin, which plays the role of carrying the oxygen that we breathe in, to the various tissues of the body.White Blood Cells :
White Blood Cells are the defense mechanism of the body. Whenever the body is subjected to attacks from outside, WBCs swing into action and protect the body. They identify, destroy and remove any foreign material that has entered the body.Platelets :
Platelets are cells, which play the role of helping in clotting of blood. Whenever there is an injury platelets play a very important part in arresting the loss of blood by enabling the process of clotting.Plasma :
Plasma is the fluid part of Blood. It enables blood to flow, and plays the role of a carrier. It carries the RBCs, WBCs and Platelets. It also plays the role of carrying nutrients to the various parts of the body, and takes out the waste matter. Thalassaemia Major is a disorder, which affects the Red Blood Cells in the Blood. The RBCs are full of haemoglobin, which carry the oxygen that we breathe, to the various tissues of the body. Haemoglobin is made up of ‘haem’ (iron component) and ‘globin’ (protein component). Two Alpha and two Beta chains form globin. In the case of Thalassaemia Major, there is a reduction in the number of Beta Chains. This leads to improper globin synthesis, and lack of haemoglobin, leading to premature destruction of the RBCs. The child will not be able to carry oxygen to the various tissues of the body. This will prove fatal to the child unless it is monitored and treated properly.Is a Genetic Disorder?
Every physical characteristic and function of the human body is controlled by a pair of genes. Genes are present in every cell of our body. You have two of every kind of gene, one passed on by your mother, the other passed on by your father. One of these two genes tends to dominate and the other is recessive. The characteristic/function acquired by a person depends on which parent’s gene dominates. There could be some characteristic where the mother’s gene dominates, whereas in other characteristics the father’s gene may. Among many other pairs of genes, you have two genes that control how haemoglobin is made in each of your red blood cells.- ‘Normal’ people are normal because they have two normal genes for haemoglobin. In other words, both parents have passed on normal genes for haemoglobin.
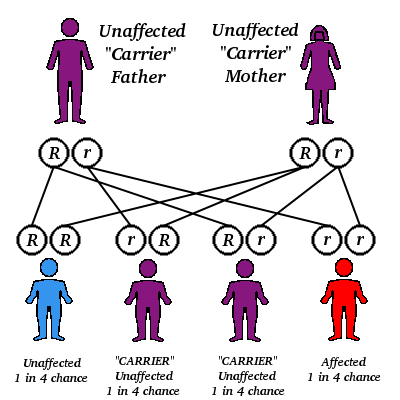
- Persons with Thalassaemia Minor (also called ‘carriers’) have one normal gene and one altered gene for haemoglobin. They are healthy because the normal gene becomes the dominant gene. One of the parents has passed on the altered gene. Therefore, atleast one parent is definitely a Thalassaemia Minor.
- People with Thalassaemia Major have two altered genes for haemoglobin. This means that both parents have passed on the altered gene. Therefore both parents have to be ‘carriers’.
If both partners in a marriage are Thalassaemia Minor, there are the following possibilities :
Causes of the ‘Altered’ Gene
Researchers have been able to identify the pair of altered genes, which cause a reduction in Beta Chains, leading to Thalassaemia Major. These genes are located on chromosome No. 11. Though it is difficult to pin-point the causes, it is clear that the genes underwent a mutation gradually over a few generations.
When one looks at the regions of the world that have a high incidence of Thalassaemia, one can see that these are the same areas that have had a problem of malaria. It is therefore being hypothesized that due to successive generations being subjected to malaria, the gene has undergone a mutation due to successive generations being subjected to malaria. This hypothesis has gained ground also because of the fact that people carrying the altered gene are known to have a lesser risk against malaria.
In short, many successive generations of the population being subjected to malaria has resulted in a genetic mutation. The ‘altered’ gene now gives improper instruction leading to a reduction in ‘beta’ chains resulting in improper synthesis of ‘globin’. The consequent lack of haemoglobin results in premature destruction of Red Blood Cells, leading to inability to deliver oxygen to the various tissues of the body.
Thalassemia Minor